With increasing recognition of mental, neurological, behavioural and substanceuse disorders classified under significant public health problems, there is a perceptible shift in considering mental health and neurosciences as a good career option
Tagged as an ˜'Institute of National Importance', NIMHANS-the National Institute of Mental Health and Neurosciences-is revered as a '˜temple' of hope for accident victim survivors, trauma patients and all those battling from mental illness, depression, alcoholism, substance abuse or similar disorders. Its origin dates back to 1954 with the inception of the '˜All India Institute of Mental Health' (AIIMH), which was established to promote medical education in post-independent India.
NIMHANS today stands testimony to Karnataka's history of mental health care system, which began with the Bengaluru Lunatic Asylum, founded in 1847 under the guidance of British medical practitioner, Dr Charles Irving Smith. In 1925, the asylum was rechristened the '˜Mental Hospital' that significantly shifted the management criteria of mental problems. The old asylum or Mental Hospital on Avenue Road was eventually closed in 1936-37 and moved to the new site at Lakkasandra, atop Bangaluru's second highest hillock. More than 100 acres of land was donated by the then Maharaja of Mysore to establish the Mental Hospital, which also received significant grants from Dewan Sir Mirza Ismail. Frank Xavier Noronha became its first superintendent. He was succeeded by Dr M V Govindaswamy, a trained doctor in the Mysore Medical Service. He was instrumental in developing the Mental Hospital into an '˜open model' mental health care institution. Dr Govindaswamy, the doyen of psychiatry successfully transformed the hospital into a modern institute of mental health and neurosciences that eventually redefined itself as a first of- its-kind training and research center in India.
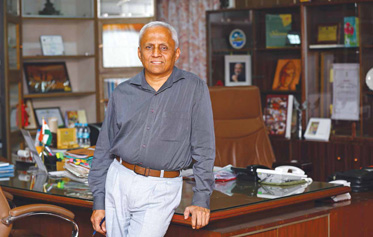
The National Institute of Mental Health and Neurosciences (NIMHANS) is considered the ‘temple of hope’ for accident victims, trauma patients and all those battling with mental illness, depression, alcoholism or substance abuse. Established to promote medical education in post-independent India, it offers holistic patient care, training and research catering to the cross-section of society, and stands as a model multi-disciplinary mental health care institution, setting the gold-standard for others. Its current mission is to get rid of the stigma and bring awareness that mental illness is like any other illness, manageable, curable, and make mental health care more accessible. In conversation with Prof B N Gangadhar, Director, NIMHANS
Dr Govindaswamy played a vital role in the formation of the AIIMH and became its founder director. AIIMH was based on the recommendations of the Health Survey and Development Committee-also known as the Bhore Committee-under the Chairmanship of Sir Joseph Bhore). Academic activities and courses in Psychiatry, Clinical Psychology and Psychiatry were introduced. Dr Govindaswamy successfully blended Indian psychology with philosophy to understand human behavior better. The amalgamation of the AIIMH and the Mental Hospital in 1974 gave birth to the National Institute of Mental Health and Neurosciences (NIMHANS). Thus, Dr Govindaswamy's vision and leadership paved the way for modern neurosurgery in this institute. He was influential in starting psychosurgery at the AIIMH. The buildings of the erstwhile AIIMH currently house the administrative sections and basic science departments of NIMHANS.
NIMHANS today carries forward the legacy of Dr Govindaswamy as a multidisciplinary haven for patient care and for academicians. It is a research and training institute to help patients conquer their mental health ailments. NIMHANS is an important aide to the central and state governments in establishing new psychiatric facilities, in improving existing facilities or for formulating a national programme on mental health. The institute provides a combination of research and training that promotes, prevents and offers curative aspects of clinical services in mental health and neurosciences. Its manpower development programme is gradually bridging the need for nurturing behavioural sciences with neurosciences and basic biological sciences with ancient health systems.

Carrying the flame of hope is its current director, Prof B N Gangadhar who assumed office in January 2016. Equipped with an MBBS degree from the Bangalore Medical College in 1978 and an MD Psychiatry degree from NIMHANS in 1981, he joined the institute as a faculty in 1982. With over 30 years of experience in the field of mental health, in both clinical and academic aspects, he served the institute in various capacities such as Medical Superintendent; Head-Department of Psychiatry; Dean Behavioural Sciences and Program Director/Head of Advanced Centre for Yoga. He was conferred the prestigious Fellow of the National Academy of Medical Sciences (FAMS) degree in 2006 and DSc (Doctor of Science) from SVYASA Yoga University, Bengaluru for his research work on Yoga and Mental Health in 2012. He is also a recipien of the coveted Sir C V Raman award and '˜Doctors Day' award from the Government of Karnataka. He also shares over 25 awards with other primary recipients.
Prof Gangadhar spoke to Corporate Citizen on the changes needed to popularise the agenda that mental illness is like any other disorder that can be treated by doctors and medicines and on the challenges and goals to reduce the severity of mental illnesses, increase accessibility of treatment and ensure better cure.
Prof Gangadhar : Before NIMHANS, the All India Institute of Mental Health (AIIMH) was recognised as a multi-disciplinary service, as a research and academic facility with the distinction of even establishing ancillary departments such as biochemistry, biostatistics, social work etc. It took a holistic stand on problems related to the mind and brain and the nervous system. In this, NIMHANS mirrored global thinking in its initial years and now continues to be a multidisciplinary organisation which makes it unique. The central government is now modelling other mental health institutions on the lines of NIMHANS as '˜NIMHANS-like' institutions.

The AIIMH was started in 1954 for promoting medical education in post independent India and was based on the recommendations of the Bhore Committee (1943-46). Three institutions were proposed - the All India Institute of Medical Sciences in Delhi, the All India Institute of Mental Health in Bengaluru and the All India Institute of Hygiene and Public Health in Kolkata. The Bhore Committee was of a singular opinion that the Mental Hospital in the erstwhile Mysore State was a progressive institute, which had developed itself as a centre for excellence and comparable with reputed international institutes. The Mental Hospital was a leader in its own right across the Indian subcontinent for adopting innovative and cutting edge technology and services for patient care even in those days-and compared very well with several leading mental health institutions globally. Hence, it was a natural choice for establishing a post graduate center in Independent India for promoting mental health human resources for the new nation (based on training gained by Dr M V Govindaswamy, at Maudsley Hospital in London in the 1930s).
The founding of NIMHANS in 1974 cemented and strengthened the existing links and bonds between the Mental Hospital and the AIIMH. Several administrative differences existing between the two institutions were ironed out and uniform standards of administration and management were brought in. This was reflected in better service delivery and enhanced patient care. Many more post graduate courses were also initiated.
NIMHANS is a pre-eminent institution for mind, brain and behavioural therapy in the country. It is multi-disciplinary and provides integrated management for care and rehabilitation. It uniquely combines neurosciences (which includes neurological and neurosurgical services) along with comprehensive mental health care (child, adolescent, adult and elderly care). The departments in the institution run super-specialty and subspecialty clinics and services. Nearly two-thirds of the patients belong to the poorer sections of the society and all obtain the same cutting edge technology and advanced patient care services at minimal or no cost. The hallmark of our innumerable teaching programs is that they are cross disciplinary activities. A recent initiative has been on developing self-sustained laboratories and services along with translational research and novel product development for diagnosis and care. The combination of service, research and academics in its right proportion is a unique and key distinguishing feature at NIMHANS which has enabled the growth and development of the institute. Successive directors of the institute have provided able leadership and nurtured a noteworthy work culture.
There is need of bringing public awareness that mental illness can be treated and a good amount can be cured. Even in people who don’t get completely cured, if they continue to take medicine they can keep their illness at bay. It is only a very small fraction of patients that get eternally hospitalised, which is often depicted in mainstream cinema

The growing numbers of patients seeking help at NIMHANS reflects on the increasing confidence. The steady growth in research publications from NIMHANS and the generation of research grants on competitive applications is another measure of success. The excellence in performance of the professionals trained at the institute bears testimony to its training standards. A harmonious work culture is the basis for this success. Naturally the government and other agencies trust NIMHANS and extend their necessary support.
Health Sciences education in mental health is at the crossroads. With increasing recognition of mental, neurological, behavioural and substance use disorders classified under significant public health problems, there is a perceptible shift in considering mental health and neurosciences as a good career option.
NIMHANS is widely recognised as an institution of high academic standards which has been maintained right from its inception. Post its deemed university status in 1994, it brought in systematic changes in framing the curriculum for post-graduate courses in mental health and neurosciences. NIMHANS was able to offer the highest available qualification of MCh (post MS qualifications) and DM degrees (post MBBS) along with an option for an integrated undergraduate programme. Additionally, doctoral research received a greater fillip. Administrative freedom allowed faster and able completion of academic tasks.
Availability of psychiatrists is not as common in rural areas because the number of psychiatrists cannot reach out to all the districts. As with other speciality doctors, psychiatrists too find practicing in urban areas more attractive
The growing numbers of patients seeking service with diverse expectations (including provision of help for their stay, diverse language and dramatic recovery) is a challenge on a day to day basis. NIMHANS has to tackle several legal battles too from time to time.
NIMHANS, as a premier institution, has been proactively interacting with the state and central governments. It has also been able to influence standards and processes of health care, policy development and programme and planning. Historically, NIMHANS has contributed to the development of the National Mental Health programme by developing community mental health initiatives and subsequently the Bellary Mental Health programme that metamorphosed into the District Mental Health Programme which is the flagship programme for mental health care in India. The institution has actively collaborated and advocated for the right of the mentally ill and their families; being a recognised centre for injury prevention and safety promotion.
NIMHANS is a leading advisor for the different state and central governments on road safety and suicide prevention. It has actively contributed and facilitated dialogue for the development of the National Mental Health Policy, new Mental Mealth Care Bill and also amendment to mental health related legislations like Narcotic Drugs and Psychotropic Substances Act, 1985 (NDPS) and Cigarettes and Other Tobacco Products Act (COTPA). The strategy of life skill education as a health promotion measure and the development of psycho-social services during and after disasters emanated from NIMHANS. Being a member of the Karnataka State Mental Health Authority, NIMHANS has influenced and helped establish the fixed day strategy for mental health service across all public health care facilities in Karnataka through its Manochaitanya programme. Currently the institution is coordinating with the Medical Research Council, UK, and ICMR, Indian Council of Medical Research, India, on collaborative research projects on non-communicable diseases and mental health in the Indian population. The activities under this Endeavour include genetic studies and also provide for longitudinal follow up of individuals who are vulnerable to mental and substance-use problems. The ancient science of yoga has been researched and its effect on promoting mental health and managing mental and substance use disorders has resulted in its inclusion into routine protocols of best clinical practices.

In both the places, communities do have an understanding and it has grown. In urban areas they tend to seek help but in rural areas although they want to seek help, they might not have access to specialised help. In rural areas, they also have other explanations for mental illness and resort to rituals etc. The availability of psychiatrists is not as common in rural areas because the number of psychiatrists cannot reach out to all the districts. As with other specialty doctors, psychiatrists too find practicing in urban areas more attractive. It is not that psychiatrists are scarce in rural areas but all specialty doctors too are scarce in rural areas. Not just NIMHANS, now the government has proposed that the curriculum of the MBBS doctor needs to be enhanced and that these doctors should be empowered to address questions on mental health. We believe that medical doctors can address many simpler common mental disorders. In the training module for the district mental health programme, my belief is that psychiatry care has to be reached out by primary care centers.
We have a department of social work and department of mental health education that periodically produce manuals, newsletters and small documentary films and programmes from time to time that have educated the general public. We broadcast several awareness programmes on Doordarshan and other TV channels. We also have collaboration with the district mental health programmes with several other states. We have extensive contact with the community across various states that educate people, train professionals to increase their capacity in the health services to enable them to meet this challenge.
The recently completed NMHS stands out as the second largest mental health survey globally and is also the most systematic and scientific study undertaken in post-independent India across 12 states covering nearly 40000 people. This unique Endeavour was undertaken with the support of the Ministry of Health and Family Welfare, Government of India. The survey has resulted in a detailed and comprehensive assessment of the systems / facilities / resources for mental health care in the surveyed states and also developed the local capability of the institutions who participated in the survey in the area of psychiatric epidemiology.
The department of Neurology has been consistently recognised for the 3rd year in a row as a premier prestigious institution for excellence in academics in Neurology in the country. The Ministry of Social Justice and Empowerment has recently awarded NIMHANS the '˜Vayoshresta Samman' for excellence in research related to the elderly. NIMHANS in the recent past has established research and academic links with globally reputed organisations / academic centres of excellence including the World Health Organisation, Royal College of Psychiatry, Fogarty Foundation, John Hopkins University, University of Liverpool, Massachusetts Institute of Technology, University of Florida, and Taipei Medical University, Maastricht University, and many more. NIMHANS has been recognised at the national level for the establishment of two centres of excellence under the DBT scheme (Fellowship).
Historically, NIMHANS was established to catalyse post-graduate training in mental health education. Continuing its mandate, it has developed and has evolved into one of the largest training institutions in mental health for formal programs and also for short term courses. Additionally, it continues to mentor the centers of excellence formental health education. It started the development of the scheme for supporting training of mental health professionals of the Government of India and is currently involved in the implementation of this programme. NIMHANS also exploits technology and employs tele-education to build capacities across the country.
The recent National Mental Health Survey 2016has once again brought to the fore the gross deficiency of mental health professionals which includes psychiatrists, psychologists, and social workers. While the attempts to train general health professionals continue, the need and demand for specialised mental health human resources vis-a-vis global standards continue torise. NIMHANS thus would be in the forefront of mental health science education. The traditional focus of mental health science education has been on cure and care in a limited manner, but the emerging domains of prevention and promotion would help to make a positive impact on the society.

There needs to be availability of psychiatric help from primary care doctors at the very basic Primary Healthcare Centres (PHCs). It should be like how we can consult our General Practitioner(GP) for an abdominal pain, knee pain or conjunctivitis without having to go to an orthopaedicor an ophthalmologist. My GP should have the ability to do the same. There is a need for more faith and ability on the primary care doctors at primary health centers. Likewise, for any mental condition, I should be able to consult my local GP and he should be equipped well to treat my condition. One main change is to understand that mental illness is like any other ailment. There has to be availability of medicines that are essential for psychiatric care at the PHCs. Patients should be made aware of their availability and that PHCs can have mental health related care or medicines. Also, medicines should be made available at PHCs to reduce the morbidity of the illness. There is need of bringing public awareness that mental illness can be treated and a good amount can be cured. Even in people who don't get completely cured, if they continue to take medicine they can keep their illness at bay. It is only a very small fraction of patients that get eternally hospitalised, which is often depicted in mainstream cinema. The occurrence is a very small fraction which is true for any disease, and it could be so with mental illness too.
We don't harvest organs here though we get a lot of accident victims at NIMHANS. As we do not have a cardiology set up or a nephrology unit or ophthalmology set up, we do tell the patient's family that we can maintain the patient on ventilator and help them to go to the relevant hospitals where they can harvest the organs. But motivating patients and family in that situation is very difficult. If this hospital had all the other facilities it could be easier to motivate to harvest and use the organ on the next patient.
Incorporating or practicing Yoga can help beat stress. This in turn can reduce the potential of developing any sort of mental illnesses, depression or alcoholism. Just as any positive lifestyle measure gives protection, for mental disorder, taking the right medicine can actually help patients to fare better. Patients can get better with medicines which are inexpensive and safe. Managing food habits and treating other ailments alongside psychiatric treatment does not interfere with the treatment.
By Sangeeta Ghosh Dastidar